Complex regional pain syndrome (CRPS) is not a well-known condition. Few doctors have heard of it, and even fewer patients. Therefore, it is not easy to get an accurate diagnosis and even harder to get appropriate treatment for this extremely painful condition.
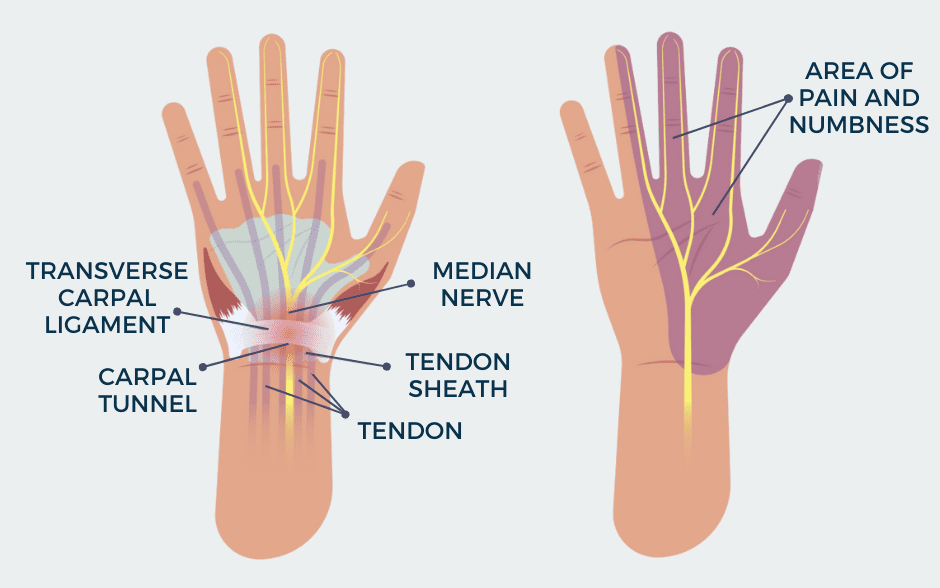
CRPS is a condition ranked highest on a pain scale developed by two Canadian doctors, Dr. Welasco and Dr. McGill. The scale has 50 points, where 0 means no pain and 50 means the highest possible pain. On this scale, CRPS is ranked 46th, while, by comparison, limb amputation is 39th and chronic migraine – 29th. Pain always occurs in one of the extremities and can be a result of an injury, such as a fracture or dislocation, a poorly performed operation, but can also be the consequence of a stroke or heart attack. In 90% of cases, it is not related to nerve damage and is called CRPS type 1. Remission is likely if the diagnosis has been made and treatment started within the first three months of the onset of symptoms. However, in 10% of cases, a nerve is damaged – it is known as type 2 CRPS and is incurable.
Typically, pain is very severe and disproportionate to the injury sustained. Other symptoms include burning and stabbing sensations of varying intensity, hypersensitivity to touch or cold, and swelling. Characteristic also are temperature fluctuations in the affected limb, together with a change in the color and texture of the skin, which may become thin and shiny. Muscle spasms, tremors, weakness, and, in time, atrophy occur. In many cases, it can go into remission however, it is incurable in 10% of people.
Dorothy’s story
Dorothy was diagnosed with CRPS type 2 in December 2019. Her story began a few months earlier, in April 2019, with a trivial accident when she fell into a hole in the sidewalk on her way to work and twisted her ankle. An ER doctor diagnosed the fracture and referred Dorothy to a surgeon for consultation. Based on the X-ray, the surgeon decided to operate and fuse the bone with metal plates and screws. The doctor expected Dorothy to return to work and have an active life three months after the procedure. Unfortunately, it has been almost three years, and that has not happened.
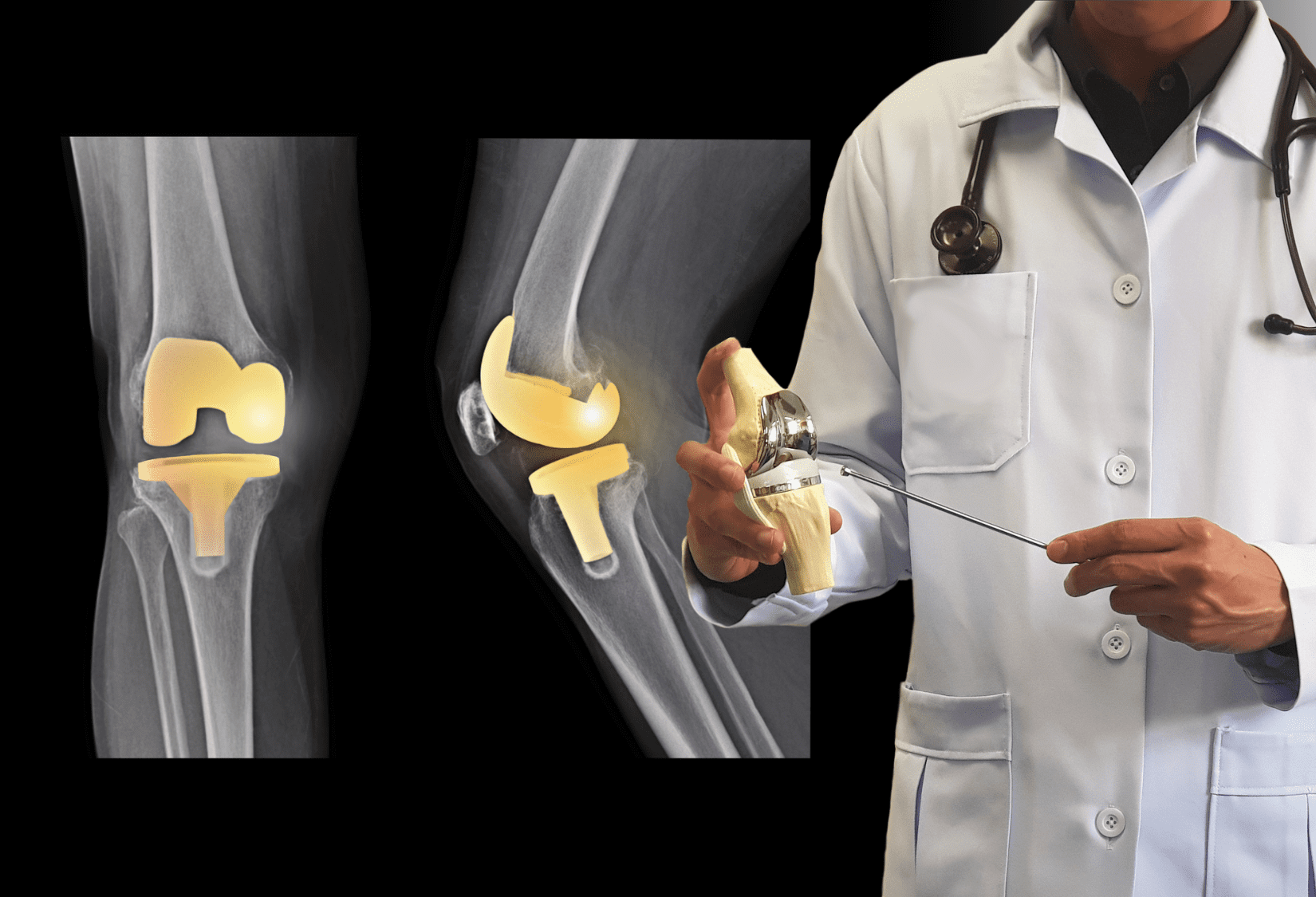
According to the doctor, the procedure went well, but the post-operative pain never went away and got worse as time went on. Unfortunately, the surgeon ignored the obvious signs and symptoms – the numbness in her leg, the burning pain, and the tingling sensation that resembled an electric shock – that something was wrong. Dorothy felt worse and worse every day, but she had no idea what was happening to her, and her doctor thought everything was normal. The pain became unbearable, so she went to her family doctor, who referred her to a neurologist. A nerve conduction study results were devastating- it showed the sensory-motor damage to 4 nerves in the leg caused by the surgery. Dorothy was diagnosed with traumatic neuropathy which was a result of the surgical intervention and referred to a pain management doctor who additionally diagnosed her with CRPS type 2. The doctor recommended a treatment consisting of three elements: three Lumbar Sympathetic Blocks every two weeks, intensive physical therapy, and medications.
The injections proved to be a lifesaver. Dorothy had managed to take two injections before the pandemic and was beginning to believe that the disease was manageable. However, the closure of hospitals and doctors’ offices in March 2020 halted the treatment. The pain seemed to start getting worse again. When medical facilities reopened, her doctor decided to perform surgery to remove metal from her leg and attempt nerve repair. The decision to have another surgery was difficult, but at this stage, the pain was already at such a level that she would do anything to make it go away.
The surgery went without complications, and she went home the same day with a pain medication pump connected to her leg. However, when the medication ran out, she began to feel very bad. She felt like someone was cutting off her leg, hammering nails, crushing, and squeezing. The pain was unbearable. “Imagine having your toes cut off. Painful, right? Now imagine having your toes cut off every second of every day for the rest of your life, constantly reliving that pain. That is what CRPS is like.” – Dorothy said about her disease.
The surgery did not change much in terms of pain levels, but Dorothy started regaining the range of motion in the ankle, and persistent swelling was diminishing. From an orthopedic standpoint, there was nothing more that could be done. Dorothy began searching on her own for information about available treatments. She found a pain management specialist who decided to start neuromodulation treatment and connected a Sprint PNS stimulator to her leg. Unfortunately, her doctor had to disconnect the stimulator after a few months due to infection. The last resort treatment was a spinal cord stimulator, an implant that disrupts the pain signals traveling between the spinal cord and the brain. The stimulator significantly reduced the pain level, but her leg needed intensive rehabilitation. She still dreamed that she would be able to return to an active life eventually, so she started looking for a physical therapist who could help her.
Unfortunately, several attempts at rehabilitation at different clinics did not result in any improvement. The therapists had never heard of CRPS and were unable to help using traditional physical therapy techniques. Dorothy did not give up. After reading several articles about the revolutionary Strain Counterstrain manual therapy technique, she decided to find a specialist who had knowledge and experience in this method. On a website listing specialists certified in Strain Counterstrain treatment, she found the name of physical therapist Piotr Domagala, owner of the PDR Physical Therapy & Wellness Center clinic. “Once again, the light in my dark tunnel has been turned on. I hope it will shine forever,” Dorothy said.
After the first session, she noticed a difference in her pain levels, which gradually decreased with each visit. Dorothy began to be more active, walking longer than before distances each day on her own. The Strain Counterstrain technique proved to be a breakthrough in treatment – this non-invasive method can bring spectacular results for CRPS patients.
“I strongly believe that the Strain Counterstrain technique should be an integral part of the treatment of CRPS because of its effects not achievable with other therapeutic techniques and its non-invasiveness. It helped me in the late stage of the disease; I think that people at the earlier stage can have excellent results and may not need a spinal cord stimulator,” she added. Although Dorothy’s disease is impossible to cure, Strain Counterstrain gives her hope of returning to her previous lifestyle.