Bionics in Medicine: How Artificial Joints Restore Mobility and Independence
Bionics in medicine — the replacement or support of organs and body parts with devices that closely imitate natural function — is advancing rapidly. Thanks to breakthroughs from scientists and clinicians, people injured in accidents or affected by degenerative diseases now have renewed hope for returning to their previous lifestyle, independence, and mobility. In addition, each year brings innovations that make these solutions more accessible and effective.
Cochlear implants that receive sound, process it, and stimulate the auditory nerve have been used successfully for years. In fact, a bionic eye has already helped a patient in the United Kingdom regain useful vision. Researchers are developing bionic muscles and limbs with natural-like range and precision, and even exploring bionic organs — more efficient lungs, durable hearts, and supportive liver technologies. Meanwhile, a bionic spine project at the University of Melbourne underscores how fast this field is growing. However, before thought-controlled limbs become common, bionics already improve daily life in everyday ways — such as replacing damaged joints so people can walk, sleep, and move without relentless pain.
What Are Bionics in Medicine?
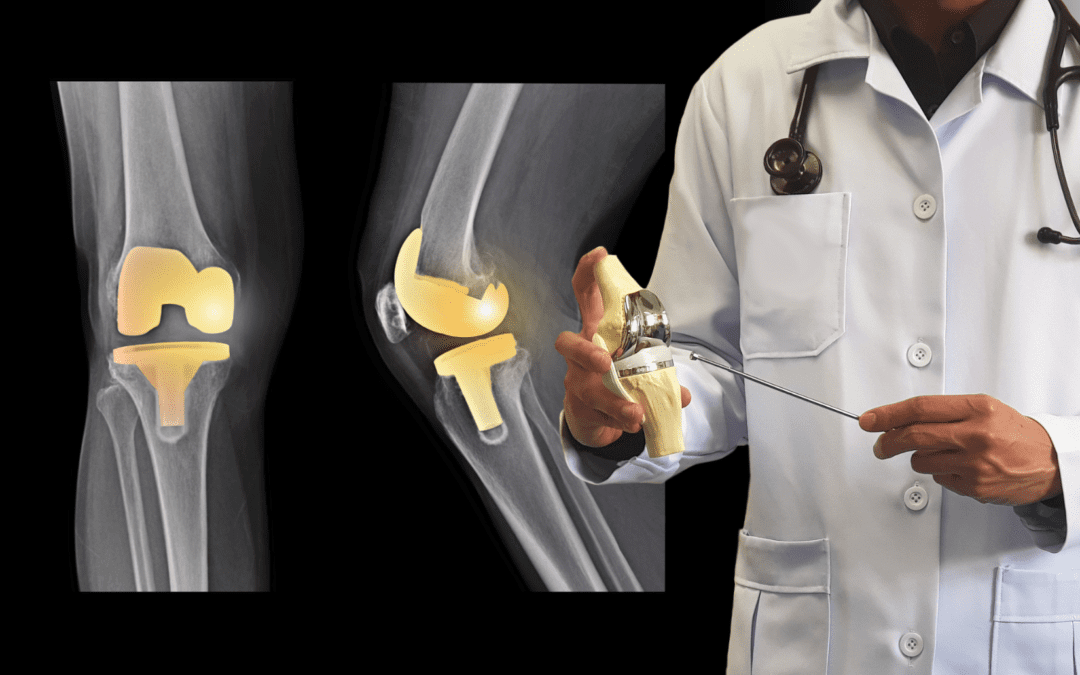
In everyday rehabilitation, “bionics” often refers to joint endoprostheses — engineered implants that replace worn or damaged cartilage and bone surfaces to restore stable, pain-free motion. These bionic joint replacements are precision-designed to mimic the biomechanics of the original joint, allowing patients to regain mobility with the support of structured, individualized physical therapy. As a result, many people return to activities they once believed were permanently out of reach.
“Bionic People” Are Among Us
As physical therapist Eva Kręcisz from PD Rehab in Mount Prospect notes, people with prosthetic limbs and joint endoprostheses are increasingly common. In the United States alone, surgeons perform more than a million hip and knee replacements each year. Although most patients don’t think of themselves as “bionic,” their modern implants clearly demonstrate how medical innovation improves quality of life. Moreover, this technology continues to evolve.
Which Joints Are Most Commonly Replaced?
Surgeons can reconstruct many joints. The most frequent include:
- Hips and knees (most common)
- Shoulders and ankles
- Fingers, elbows, and other smaller joints
For many, joint replacement ends months or years of pain and progressive disability. When non-invasive options are exhausted and pain limits walking, sleeping, or dressing, a bionic joint replacement offers a path back to normal functioning. Furthermore, the long-term success rate remains high when patients follow a structured rehabilitation plan.
Preparing for Surgery: Preoperative Physical Therapy
Targeted prehab strengthens the right muscles, teaches safe movement strategies, and speeds recovery. For example, your therapist may help you:
- Strengthen key muscles to support the new joint
- Learn crutch/walker use and safe stair negotiation
- Practice essential transfers (bed, chair, toilet) when knee/hip motion is limited
What Happens After the Procedure?
Early movement and a structured rehab plan drive long-term results. Patients who actively participate in therapy typically regain function faster and maintain it longer. In contrast, people who stop too early often struggle with lingering stiffness and weakness. Many “unsuccessful surgeries” are really rehab problems — insufficient mobility work, inadequate strength training, or stopping therapy too soon. Therefore, consistent follow-through is essential.
Your Post-Surgery Rehabilitation Roadmap
- Comprehensive evaluation: pain level, range of motion, gait, daily activities
- Manual therapy and mobility work to reduce stiffness and swelling
- Progressive strengthening and balance training for safe, confident walking
- Home exercise program with clear milestones to protect the new joint
Home Health Support in the First Weeks
Many patients receive short-term home care right after discharge. During this time, they may see:
- A nurse and physical therapist visiting for about two weeks
- Support with vitals, medications, and gentle rehab
- A smooth transition to outpatient post-surgical physical therapy
Real-World Results: Life After a Bionic Joint
At PD Rehab in Mount Prospect, we routinely see patients return to hiking, traveling, and playing with grandkids. One patient, Mary, has replacements in a hip, a shoulder, and both knees. With consistent, well-paced therapy, she walked around an island in Portugal and later sent a photo captioned: “My new hip climbed to the top of this mountain!” Stories like hers show how modern bionic joint replacement, combined with quality rehabilitation, restores comfort, mobility, and confidence. Finally, for many people, this technology becomes their path back to a full, active life.
Ready to Regain Your Mobility?
Whether you’re preparing for joint replacement or recovering after surgery, our physical therapy specialists at
PD Rehab in Mount Prospect can help you move safely and confidently again. We combine advanced manual therapy, individualized exercise programs, and gentle techniques to support your recovery every step of the way.
Read more about our post-surgical physical therapy, how we treat with Fascial Counterstrain, and managing adhesions and scar tissue.