Bionics in medicine, i.e. the replacement or support of various organs and body parts with devices that closely imitate their natural functioning, is a relatively new phenomenon that is, however, rapidly gaining popularity. Through scientists’ work and knowledge, many people injured in accidents or as a result of various diseases gain hope for returning to their previous lifestyle and mobility.
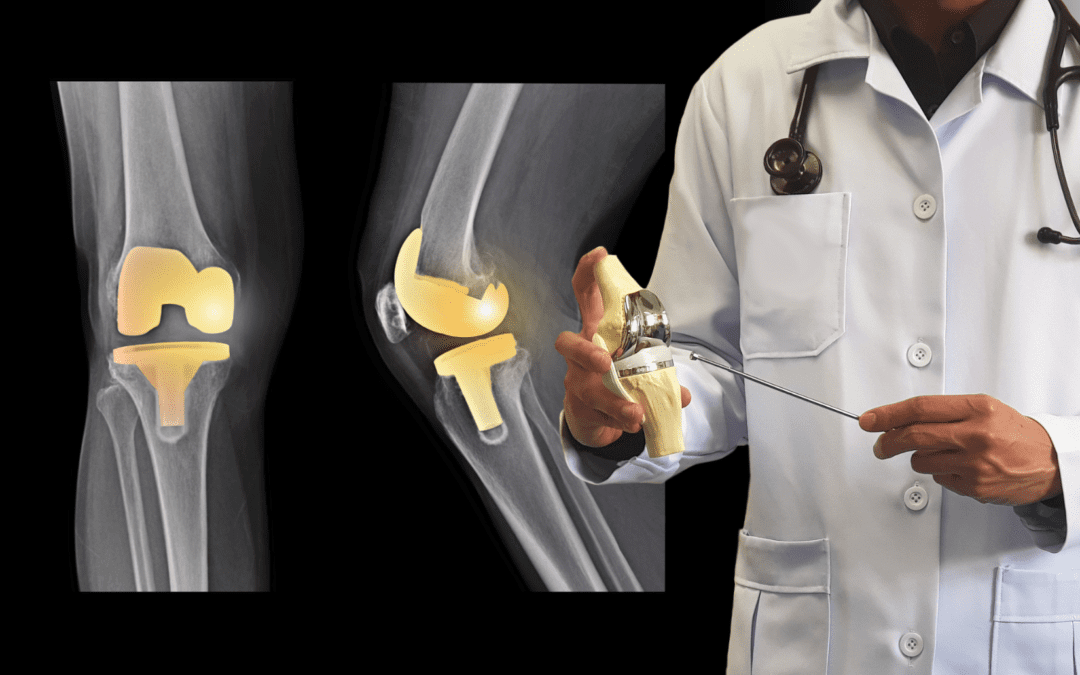
A cochlear ear implant that receives sound, processes it, and electrically stimulates the auditory nerve has been successfully used on the market for years. A patient in the United Kingdom was successfully implanted with a bionic eye that helped him regain his sight loss due to a serious illness. Scientists are trying to create bionic muscles and limbs whose range of motion and precision would be identical to natural limbs. They also work on bionic organs – more efficient lungs, an indestructible heart, or a liver. Substantial hopes are also being placed on the bionic spine, which neuroscience experts and biomedical engineers at the University of Melbourne are working on. Bionics provides enormous promise for humankind to remain healthy and fit even after a serious illness or unfortunate accident. But before we get to thought-controlled limbs, we may need the help of bionics for more trivial matters, such as replacing damaged joints. There are already quite a few people among us today who have just regained their lost mobility thanks to bionics.
About the use of bionics in joint disease we talk today with Eva Kręcisz, a physical therapist at the PD Rehab clinic in Mount Prospect.
Eva, is it true that bionic people are living among us?
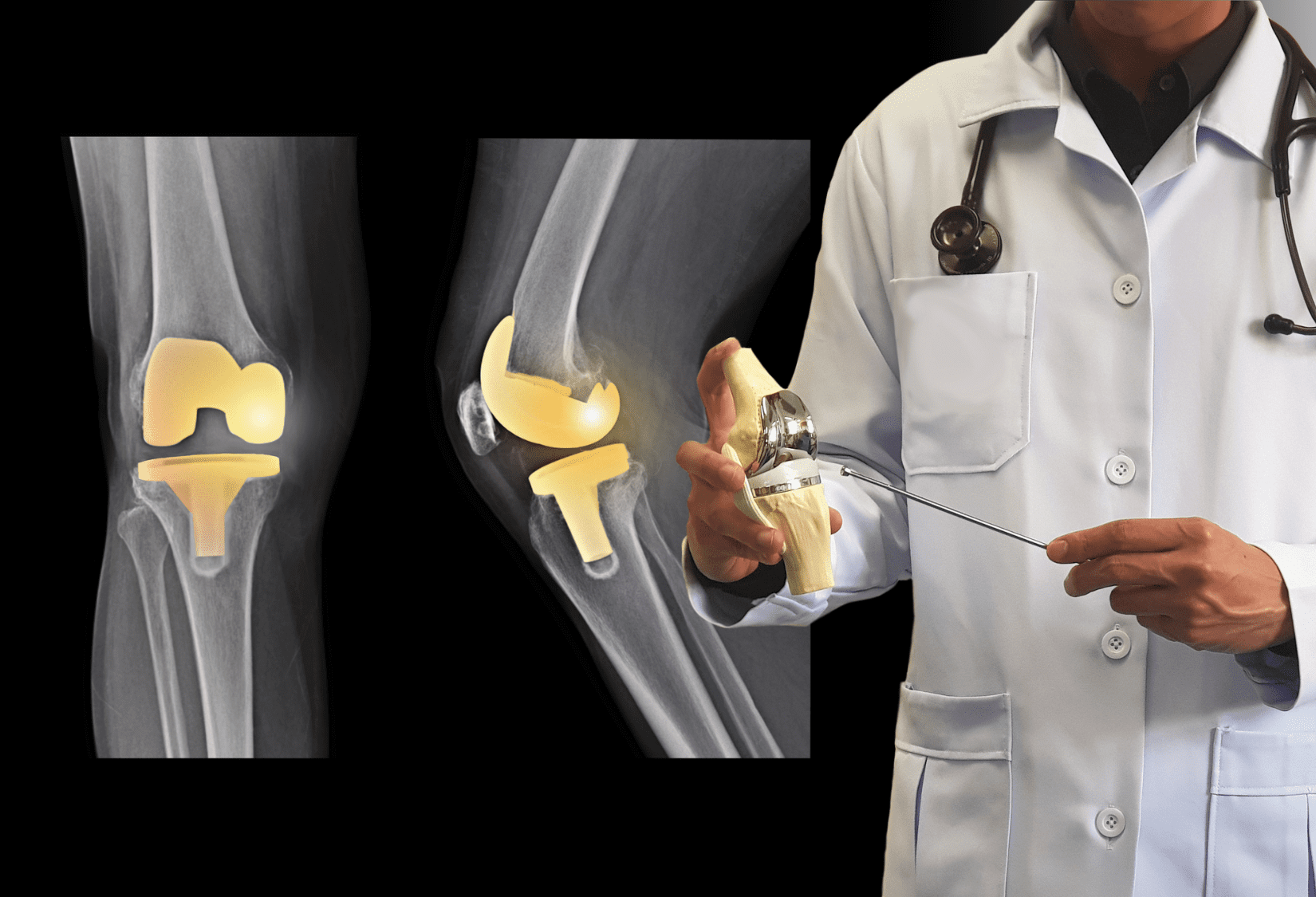
Eva: Yes, and there are more and more of them! I am talking about those who have prosthetic arms or legs after limb amputations, as well as those who have endoprostheses (internal prostheses) after joint replacements. In the United States alone, there are over a million hip and knee replacements a year. Bionic people are among us, although they probably do not think about themselves in this way.
What joints are most commonly replaced?
Surgeons can reconstruct almost all joints – the most common are hip and knee replacements, besides shoulders, ankles, and even fingers. I had a patient who had part of his elbow joint replaced after an accident. One of our patients, Maria, has already had a hip, shoulder and both knees replaced. She is pleased with her decision to have the procedures done. Although it is a radical solution, for most patients the joint replacement ends months or years of living in pain and progressive disability. When other non-invasive methods have been exhausted and pain greatly limited walking, sleeping, or dressing, a joint transplant offers a chance to return to normal functioning.
Is there any preparation necessary for this kind of surgery?
Of course. Pre-operative physical therapy is very important. A therapist knows which muscles should be strengthened to make it easier to move after the surgery and speed up the recovery and prepare an adequate treatment plan. Patients learn how to walk on crutches or use a walker, how to descend stairs safely if they cannot rely on an operated leg, and even how to sit down and get up from the toilet if a knee or a hip will not bend. Such trivial activities do not cause us any problems when we are fit but after the surgery, they become a real challenge.
What happens after the procedure?
As a patient leaves the hospital, he or she should look for a good physical therapy clinic. In my experience, those individuals who have exercised and actively participated in the rehabilitation process have the best long-term results. Neglecting rehabilitation leads to chronic pain because the knee, shoulder, or ankle does not return to full function. A large number of so-called unsuccessful surgeries are related to improperly conducted or lack of postoperative rehabilitation.
After surgery, can the patient count on some help at home before they can function pretty normally?
Absolutely. For a few weeks, a nurse and a therapist come to the house. Usually, home health care lasts two weeks. They check vitals, and medicines, and slowly start rehabilitation. The next step is attending a post-surgery rehabilitation program in an outpatient physical therapy clinic. A patient needs to be evaluated as to pain level, and range of motion in the operated joints. Therapists also check if and how the patient can perform daily activities. Based on this, a plan of care is prepared with the main goal of helping the patient to return to full mobility as quickly as possible. Our therapists also try to encourage the patient to exercise regularly and reasonably so that they can enjoy their new joint for as long as possible without complications. I have to say that it gives me great satisfaction to hear stories of how the new knee allowed Maria to walk around an entire island on a trip to Portugal, or when I get a photo from the mountains with the caption “My new hip climbed to the top of this mountain!” So let’s not be afraid of joint implants, they can improve the quality of our life and let us enjoy it once again.
If you are facing joint replacement surgery, plan your pre- and post-operative physical therapy for a quick recovery. Call us or click here to schedule your complimentary consultation with one of our experienced specialists.